Take action
Add your name to our open letter to the Federal Minister for Health
Australians are calling on the federal government to:
- Recognise chronic UTI as a legitimate medical condition, with a standardised definition.
- Review outdated testing and treatment—conduct a national review of current UTI testing methods and clinical guidelines.
- Update guidelines and education—revise clinical guidelines and train healthcare professionals in up-to-date, evidence-based UTI care, including for chronic embedded infections.
- Fund research—provide dedicated government funding for chronic UTI research, including the development of better diagnostic tests and faster, safer treatments.
- Establish one or more specialist clinics—create multidisciplinary clinics across Australia to treat chronic and complex UTI and support other healthcare providers to care for these patients.
Read the full letter...
Minister for Health and Aged Care
Parliament House
Canberra ACT 2600
By email: ministerbutler@health.gov.au
Dear Minister,
Re: Urgent need for recognition and reform in the diagnosis and treatment of chronic urinary tract infection
We represent a large and rapidly growing community of Australians affected by urinary tract infection (UTI). Our letter outlines the experiences of thousands of Australians—predominantly women, and also some men and children—who have had their lives derailed by chronic UTI.
The actions we request from the Government have been identified by Chronic UTI Australia[1]—the nation’s only patient advocacy group dedicated to UTI—based on extensive patient liaison and surveys; monitoring of relevant scientific literature; and communication with researchers and medical experts, both in Australia and internationally.
What we are asking the Federal Government to do
We are asking the Government to implement the following actions as a matter of priority:
- Recognise chronic UTI as a legitimate medical condition, with a standardised definition.
- Review outdated testing and treatment—conduct a national review of current UTI testing methods and clinical guidelines.
- Update guidelines and education—revise clinical guidelines and train healthcare professionals in up-to-date, evidence-based UTI care, including for chronic embedded infections.
- Fund research—provide dedicated government funding for chronic UTI research, including the development of better diagnostic tests and faster, safer treatments.
- Establish one or more specialist clinics—create multidisciplinary clinics across Australia to treat complex UTI, including chronic UTI, and support other healthcare providers to care for these patients.
What is chronic UTI
Chronic UTI is caused by the parasitisation of bladder wall cells by intracellular microbes and microbial biofilms. Put simply, chronic UTI is an embedded bladder infection.[2]
Chronic UTI is a very painful and debilitating condition that has been long neglected by the health system and in medical research. In February 2025, the Urological Society of Australia and New Zealand (USANZ) formally recognised chronic UTI as a distinct condition that may be undetected by standard urine tests.[3] This followed an article in Medical Journal of Australia Insight calling for an urgent paradigm shift in UTI diagnosis and recognition of chronic UTI.[4]
Chronic UTI is not rare or random. It is a consequence of routine failures in the diagnosis and treatment of a common bacterial infection that affects at least half of all women at some point in their lives. As we explain below, healthcare professionals often mistake chronic UTI for non-infective bladder conditions, leading to inadequate recognition and treatment.
What is the problem diagnosing chronic UTI?
A robust body of scientific evidence shows that currently used urine tests—urinary dipsticks and the ‘gold standard’ mid-stream urine (MSU) cultures—are not fit for purpose and miss a large proportion of infections.[5] [6] [7] [8] Once bacteria become embedded in the bladder wall and form biofilms—hallmarks of chronic UTI—culture tests are almost entirely useless.[9] [10] Hence, more than 90% of participants in Chronic UTI Australia’s 2023 Hearing Patient Voices survey had received a negative urine culture result while symptomatic.[11]
Most Australian health professionals are unaware of the inadequacies of standard UTI tests, as the various UTI clinical guidelines that exist in Australia ignore the known failures of current testing tools.
Although the limitations of the tests are well recognised by scientists, researchers struggle to secure funding to solve the problem and stem a growing health crisis.
What is the problem with UTI treatment?
On the basis of the outdated and insensitive diagnostic methods, patients are often denied treatment for their infection despite having clear clinical signs and symptoms.
Further, Australia’s current clinical guidelines for UTIs fail to offer evidence-based advice for doctors treating recalcitrant UTI (that is, persistent recurrent and chronic UTI).[12] Patients are frequently prescribed low-dose antibiotic regimens or short antibiotic courses that were designed to treat acute infections. These management approaches may allow bacteria to persist and embed in the bladder wall, rendering future diagnosis and treatment more difficult. [13] [14] [15] [16] This can lead to life-altering physical and mental health impacts and the risk of life-threatening complications such as kidney damage and sepsis.
In Australia there are no clinics or tertiary centres specialising in the management of complex and chronic UTI. [17] These exist in some other countries, and the current situation is forcing Australian sufferers who can afford it to seek treatment overseas.
For the reasons outlined below, there is an urgent need to make accurate, evidence-based and up-to-date UTI information, education and referral pathways available to Australian general practitioners (GPs) and other doctors.
What is the impact of chronic UTI on sufferers?
Chronic UTI Australia’s Hearing Patient Voices survey of 410 Australians (97% women) living with chronic UTI reveals a stark contrast to the common perception of UTI as trivial and easily resolved. The large majority of survey participants reported experiencing:
- Excruciating, persistent pelvic pain, with an average score of 7.9 on a 10-point pain scale, and other distressing symptoms.
- Significant mental health impacts, with one in ten participants volunteering—without any prompting—that that their symptoms had led to suicidal thoughts.
- Severe disruption to relationships, sleep, work, and other life domains.
- Medical gaslighting, with over 80% saying their symptoms had been disbelieved or dismissed.
- Misdiagnoses, and unnecessary, ineffective medical and surgical interventions.
- High use of medical services: survey participants were almost three times more likely to have been hospitalised or to have seen multiple health providers in a single year, compared to the general population.[18]
What is the impact of chronic UTI on society and the health system?
The results of Chronic UTI Australia’s research suggest not only human suffering, but considerable avoidable public expenditure, as women cycle through emergency departments, GPs, and specialists—often failing to get effective diagnosis or treatment.
Critically, UTI-related conditions appear to be a growing burden on health systems.[19] [20] [21] Although there is not specific data on recurrent or chronic UTI, hospital separations for UTI-related diagnoses in Australia rose from 48,355 in 2007-08 to 70,046 in 2022-23.[22] This mirrors trends in the United States and the United Kingdom,[23] [24] and supports evidence of a worldwide increase in the health burden associated with UTI.[25] The Australian Institute of Health and Welfare has also provided data showing a disturbing threefold increase in the rate of death by urosepsis between 2008 and 2022, with most of the increase in the elderly population.[26]
Opportunity for action to strengthen the Government’s women’s health agenda
We commend the Federal Government’s recent focus and election commitments to women’s health. Chronic UTI deserves inclusion in this conversation. Chronic UTI has been recognised by international experts as an example of the ‘gender health gap’, in which conditions predominantly affecting women are neglected in research funding, medical education and healthcare.[27]
Chronic UTI Australia works in parallel with the Chronic and Recurrent UTI Support Group (Australia and New Zealand), a growing online patient community of more than 2000 members. This shows that despite the Government’s recent women’s health initiatives, patients with recalcitrant UTI still cannot access accurate information, evidence-based treatment, or specialist care in Australia. Expertise in chronic UTI diagnosis and management is not available from most Australian GPs, urologists, or the Government’s new pelvic pain clinics.
The actions outlined on page 1 of our letter would address a significant gap in the Australian health system and women’s healthcare. These initiatives would bring Australia to the forefront of international policy and practice in this area. The United Kingdom has recently officially recognised chronic UTI and has an NHS clinic dedicated to treating chronic and complex UTI, as well as several tertiary and private clinics. Many Australian chronic UTI patients—those who can afford it—are forced to seek treatment from a London-based clinic that accepts international patients, due to lack of expertise in Australia.
Our closing appeal
While recent recognition of chronic UTI by Australian health leaders is welcomed by patients, leadership from the federal government is needed to ensure it translates to meaningful changes to prevent, detect and effectively treat the condition.
We are not asking you to perform a miracle today—only properly funded science will achieve that. But people affected by chronic UTI want to be believed, properly diagnosed, and given the same access to evidence-based treatment that patients with other serious infections receive as a matter of course.
As a first step, the Government could establish a parliamentary inquiry or government consultancy to examine the information contained in this letter and develop a plan to implement the actions we have requested.
We would welcome the opportunity to meet with you or members of your Government to discuss these issues further and explore how federal leadership can catalyse meaningful change for people affected by chronic UTI. To arrange future dialogue with Chronic UTI Australia, please contact Deirdre Pinto or Andrea Sherwin using the contact information below.
Yours sincerely,
[1] https://www.chronicutiaustralia.org.au/about-us/
[2] https://www.chronicutiaustralia.org.au/wp-content/uploads/2024/12/What-is-a-Chronic-UTI-fact-sheet.png
[3] https://usanz.org.au/info-resources/position-statements-guidelines/chronic-urinary-tract-infections
[4] https://insightplus.mja.com.au/2024/30/its-time-we-recognised-chronic-urinary-tract-infection
[5] Stamm WE. Recent developments in the diagnosis and treatment of urinary tract infections https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1274066
[6] Tarnished Gold—the ‘Standard’ Urine Culture: Reassessing the Characteristics of a Criterion Standard for Detecting Urinary Microbes https://www.frontiersin.org/articles/10.3389/fruro.2023.1206046/full
[7] Reassessment of Routine Midstream Culture in Diagnosis of Urinary Tract Infection, https://jcm.asm.org/content/early/2018/12/10/JCM.01452-18
[8] Urine Trouble: Should we think Differently about UTI? https://link.springer.com/article/10.1007%2Fs00192-017-3528-8
[9] Women with Symptoms of a Urinary Tract Infection but a Negative Urine Culture: PCR-Based Quantification of Escherichia Coli suggests Infection in Most Cases, https://www.sciencedirect.com/science/article/pii/S1198743X17302094
[10] Spectrum of Bacterial Colonization Associated with Urothelial Cells from Patients with Chronic Lower Urinary Tract Symptoms, https://pubmed.ncbi.nlm.nih.gov/23596238
[11] Hearing Patient Voices: Chronic UTI Survey, https://www.chronicutiaustralia.org.au/survey
[12] A range of peer-reviewed papers describing evidence-based approaches to chronic UTI treatment is available at: https://www.chronicutiaustralia.org.au/research/
[13] Weak Antibiotic Doses Undermine our Body’s Defences, https://www.sciencenorway.no/antibiotics-bacteria-forskningno/weak-antibiotic-doses-undermine-our-bodys-defences/1391632
[14] Subinhibitory Antibiotic Therapy Alters Recurrent Urinary Tract Infection Pathogenesis through Modulation of Bacterial Virulence and Host Immunity, http://mbio.asm.org/content/6/2/e00356-15.full
[15] Sub-Lethal Antibiotic Treatment Leads to Multidrug Resistance via Radical-induced Mutagenesis, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2840266
[16] Continuous Low-dose Antibiotic Prophylaxis for Adults with Repeated Urinary Tract Infections (AnTIC): a Randomised, Open-label Trial, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(18)30279-2/fulltext
[17] A specialist clinic for the diagnosis and management of chronic and complex UTIs in children is being planned at Westmead Hospital in Sydney.
[18] Hearing Patient Voices: Chronic UTI Survey, https://www.chronicutiaustralia.org.au/survey
[19] The Increase in Hospitalizations for Urinary Tract Infections and the Associated Costs in the United States, 1998–2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5414046
[20] Antimicrobial Resistant Infections Keep Rising Despite Fall in GP Prescriptions, https://www.bmj.com/content/371/bmj.m4502
[21] Response to ‘Antimicrobial Resistant Infections Keep Rising Despite Fall in GP Prescriptions’, https://www.bmj.com/content/371/bmj.m4502/rapid-responses
[22] Australian Institute of Health and Welfare (AIHW): Data supplied to Chronic UTI Australia, June 2025.
[23] The Increase in Hospitalizations for Urinary Tract Infections and the Associated Costs in the United States, 1998–2011, https://pmc.ncbi.nlm.nih.gov/articles/PMC5414046
[24] Malone-Lee, James. Cystitis Unmasked. tfm Publishing Limited, 2021, p.124.
[25] Global, Regional, and National Burden of Urinary Tract Infections from 1990 to 2019: an Analysis of the Global Burden of Disease Study 2019, https://pubmed.ncbi.nlm.nih.gov/35066637
[26] Australian Institute of Health and Welfare (AIHW): Data supplied to Chronic UTI Australia, April 2024.
[27] Why Women are Not Treated Equally in Healthcare and What Can be Done, https://www.nature.com/articles/s41585-025-01063-1.epdf
Other ways to act

Write to your local MP

Share your story with us

Spread the word online
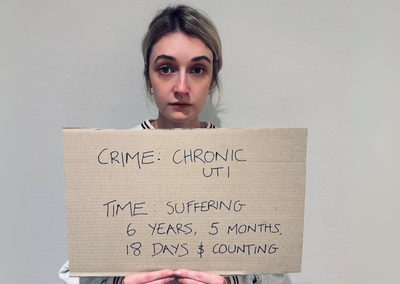
UTI photo challenge
Sign up to our email list
We provide up-to-date information and help with navigating chronic UTIs. Sign up to our email list and receive a copy of our Understanding Chronic UTI information booklet.